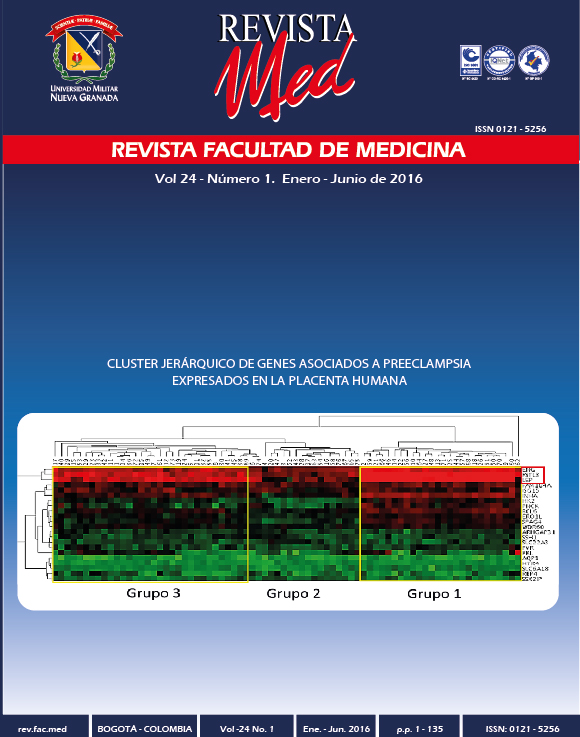
Caracterização estrutural e funcional de genes associados à Pré-eclâmpsia expressaram em humanos placenta
Resumo
Introdução: A pré-eclâmpsia ainda é a principal causa perinatal Morbi-mortalidade; devido ao avanço na aplicação das ciências “ómicas” o conhecimento sobre sua etiologia molecular tem aumentado nos últimos anos, Isto levou à identificação de genes candidatos, que estariam envolvidos na sua Patogênese.
Objetivo: Para identificar esses genes, Expresso em placenta que está associada à pré-eclâmpsia e comparar as suas características estruturais e funcionais.
Métodos: A partir de uma revisão da literatura, foram encontrados 16 genes, cuja expressão na placenta foi asociada à patología. Extração de dados Foi realizada incluindo as seguintes variáveis genómicas: Número de genes, tamanho genômico, exon contagem de codificação, CpG ilhas e repetir elementos em uma janela de 100Kbp. Para a análise bioinformática, Utilizamos diferentes recursos do NCBI (www.ncbi.nlm.nih.gov) e do UCSC Genome Browser (http://genome.ucsc.edu/).
Além disso, o portal BioGPS (http://biogps.gnf.org/#goto=welcome) foi utilizado para determinar os níveis de expressão de cada gene por tecido.
Resultados: Se encontrou diferenças significativas para os elementos não codificantes da cromatina nos genes associados, Em comparação com os controlos (teste de Kruskall-Wallis, P = 0,0341824). Os genes LEP, EBI3, PROCR, FSTL3, HEXB, INHBA e ENG foram os que apresentaram os maiores valores de z-score na placenta pré-eclâmpsica.
Conclusão: A aplicação de ferramentas computacionais tornou-se um poderoso instrumento para a análise integrada da expressão gênica e seu papel na patogênese da PE. Isso levaria a uma detecção precoce das mulheres afetadas.
Downloads
Referências
Herrera JA, Herrera-Miranda R, Herrera-Escobar JP, Nieto-Díaz A. Reducción de la mortalidad materna por preeclampsia en Colombia - un análisis de series de tiempo interrumpido. Colombia Médica. 2014; 45:25-31.
Sircar M, Thadhani R, Karumanchi SA. Pathogenesis of preeclampsia. Curr Opin Nephrol Hypertens. 2015; 24:131-138.http://dx.doi.org/10.1097/MNH.0000000000000105
Mol BW, Roberts CT, Thangaratinam S, Magee LA, de Groot CJ, Hofmeyr GJ. Pre-eclampsia. Lancet. 2015; pii: S0140-6736.
Cohen JM, Beddaoui M, Kramer MS, Platt RW, Basso O, Kahn SR. Maternal Antioxidant Levels in Pregnancy and Risk of Preeclampsia and Small for Gestational Age Birth: A Systematic Review and Meta-Analysis. PLoS One. 2015; 10(8):e0135192.http://dx.doi.org/10.1371/journal.pone.0135192
Dekker GA. Management of preeclampsia. Pregnancy Hypertens. 2014;4(3):246-247.http://dx.doi.org/10.1016/j.preghy.2014.04.021
Said J, G. Dekker G. Pre-eclamsia and trombophilia. Best Practice & Research Clinical Obstetrics & Gynaecology 2003;17(3): 441-458.http://dx.doi.org/10.1016/S1521-6934(03)00008-7
Gillon TE, Pels A, von Dadelszen P, MacDonell K, Magee LA. Hypertensive disorders of pregnancy: a systematic review of international clinical practice guidelines. PLoS One. 2014;9(12):e113715.http://dx.doi.org/10.1371/journal.pone.0113715
Kajii T, Ohama K. Androgenetic origin of hydatidiform mole. Nature 1977; 268(5621): 633-634.http://dx.doi.org/10.1038/268633a0
Hansson SR, Chen Y, Brodszki J, Chen M, Hernandez-Andrade E, Inman JM, et. al. Gene expression profiling of human placentas from preeclamptic and normotensive pregnancies. Mol Hum Reproduction. 2006; 12: 169-179.http://dx.doi.org/10.1093/molehr/gal011
Lyall F. The human placental bed revisited. Placenta 2002; 23: 555-562.http://dx.doi.org/10.1053/plac.2002.0850
Lyall F. Development of the utero-placental circulation: the role of carbon monoxide and nitric oxide in trophoblast invasion and spiral artery transformation. Microscopy Res Technique. 2003; 60(4): 402-411.http://dx.doi.org/10.1002/jemt.10278
Garoby-Salom S, Vayssiere C, Salvayre R, Parant O, Negre-Salvayre A. Oxidative stress and preeclampsia: A review. Gynecol Obstet Fertility. 2015; pii: S1297-9589.
Gram M, Dolberg Anderson U, Johansson ME, Edström-Hägerwall A, Larsson I, Jälmby M, Hansson SR, Åkerström B. The Human Endogenous Protection System against Cell-Free Hemoglobin and Heme Is Overwhelmed in Preeclampsia and Provides Potential Biomarkers and Clinical Indicators. PLoS One. 2015; http://dx.doi.org/10.1371/journal.pone.0138111
Vanwijk MJ, Kublickiene K, Boer K, Vanbavel E. Vascular function in preeclampsia. Cardiovascular Research. 2000; 47(1): 38-48.http://dx.doi.org/10.1016/S0008-6363(00)00087-0
Nishizawa H, Pryor-Koishi K, Kato T, Kowa H, Kurahashi H, Udagawa Y. Microarray Analysis of Differentially Expressed Fetal Genes in Placental Tissue Derived from Early and Late Onset Severe Pre-eclampsia. Placenta. 2007; 28: 487-497.http://dx.doi.org/10.1016/j.placenta.2006.05.010
Cox B, Leavey K, Nosi U, Wong F, Kingdom J. Placental transcriptome in development and pathology: expression, function, and methods of analysis. Am J Obstet Gynecol. 2015; 213 (Suppl):S138-151.http://dx.doi.org/10.1016/j.ajog.2015.07.046
Sõber S, Reiman M, Kikas T, Rull K, Inno R, Vaas P, Teesalu P, Marti JM, Mattila P, Laan M. Extensive shift in placental transcriptome profile in preeclampsia and placental origin of adverse pregnancy outcomes. Sci Rep. 2015; 5: 13336.ttp://dx.doi.org/10.1038/srep13336
Winn VD, Gormley M, Paquet AC, Kjaer-Sorensen K, Kramer A, Rumer KK, et al. Severe Preeclampsia-Related Changes in Gene Expression at the Maternal-Fetal Interface Include Sialic Acid-Binding Immunoglobulin-Like Lectin-6 and Pappalysin-2. Endocrinology. 2009; 150(1):452-462.http://dx.doi.org/10.1210/en.2008-0990
Enquobahrie DA, Meller M, Rice K, Psaty BM, Siscovick DS, Williams MA. Differential placental gene expression in preeclampsia. Am J Obst Gynecol. 2008; 199:566.e1-566.e11.http://dx.doi.org/10.1016/j.ajog.2008.04.020
Rajakumar A, Chua T, Handley DE, Bunce KD, Burke B, Hubel CA, et al. Maternal gene expression profiling during pregnancy and preeclampsia in human peripheral blood mononuclear cells. Placenta 2011; 32: 70-78.http://dx.doi.org/10.1016/j.placenta.2010.10.004
Su AI, Wiltshire T, Batalov S, Lapp H, Ching KA, Block D, et. al. A gene atlas of the mouse and human protein-encoding transcriptomes. Proc Natl Acad Sci USA. 2004; 101(16):6062-6067.http://dx.doi.org/10.1073/pnas.0400782101
Wu C, Orozco C, Boyer J, Leglise M, Goodale J, Batalov S, et al. BioGPS: an extensible and customizable portal for querying ang organizing gene annotation resources. Genome Biology 2009; 10(11): R130.http://dx.doi.org/10.1186/gb-2009-10-11-r130
Winn VD, Haimov-Kochman R, Paquet AC, Yang YJ, Madhusudhan MS, Gormley M, et. al. Gene expression profiling of the human maternal-fetal interface reveals dramatic changes between midgestation and term. Endocrinology 2007; 148:1059-1079.http://dx.doi.org/10.1210/en.2006-0683
Laresgoiti-Servitje E, Gomez-Lopez N. The pathophysiology of preeclampsia involves altered levels of angiogenic factors promoted by hypoxia and autoantibody-mediated mechanisms. Biol Reprod. 2012; 87(2):36.http://dx.doi.org/10.1095/biolreprod.112.099861
Jeha D, Usta I, Ghulmiyyah L, Nassar A. A review of the risks and consequences of adolescent pregnancy. J Neonatal Perinatal Med. 2015 Mar 12. [Epub ahead of print].http://dx.doi.org/10.3233/NPM-15814038
Martinussen MP, Bracken MB, Triche EW, Jacobsen GW, Risnes KR. Folic acid supplementation in early pregnancy and the risk of preeclampsia, small for gestational age offspring and preterm delivery. Eur J Obstet Gynecol Reprod Biol. 2015;195:94-99. http://dx.doi.org/10.1016/j.ejogrb.2015.09.022
Boeldt DS, Hankes AC, Alvarez RE, Khurshid N, Balistreri M, Grummer MA, Yi F, Bird IM. Pregnancy programming and preeclampsia: identifying a human endothelial model to study pregnancy-adapted endothelial function and endothelial adaptive failure in preeclamptic subjects. Adv Exp Med Biol. 2014; 814:27-47.http://dx.doi.org/10.1007/978-1-4939-1031-1_4
Murphy MS, Bytautiene E, Saade G, Smith GN. Alterations to the maternal circulating proteome after pre-eclampsia. Am J Obstet Gynecol. 2015 Oct 14. pii: S0002-9378(15)01271-5.
Monk D. Genomic imprinting in the human placenta. Am J Obstet Gynecol. 2015; 213(4 Suppl):S152-S162.http://dx.doi.org/10.1016/j.ajog.2015.06.032
Calicchio R, Doridot L, Miralles F, Méhats C, Vaiman D1. DNA methylation, an epigenetic mode of gene expression regulation in reproductive science. Curr Pharm Des. 2014; 20(11):1726-1750.http://dx.doi.org/10.2174/13816128113199990517
Ichiyanagi K, Okada N. Mobility Pathways for Vertebrate L1, L2, CR1, and RTE Clade Retrotransposons. Mol Biol Evol 2001; 25(6):1148-1157.http://dx.doi.org/10.1093/molbev/msn061
Khazina E, Weichenrieder O. Non-LTR retrotransposons encode noncanonical RRM domains in their first open reading frame. Proc Natl Acad Sci USA. 2009; 106:731-736.http://dx.doi.org/10.1073/pnas.0809964106
Schulz LC, Widmaier EP, Qiu J, Roberts RM. Effect of leptin on mouse trophoblast giant cells. Biol Reprod 2009; 80: 415-424.http://dx.doi.org/10.1095/biolreprod.108.073130
Cameo P, Bischof P, Calvo JC. Effect of leptin on progesterone, human chorionic gonadotropin, and interleukin-6 secretion by human term trophoblast cells in culture. Biol Reprod 2003; 68: 472-477.http://dx.doi.org/10.1095/biolreprod.102.006122
Schulz LC, Widmaier EP. The effect of leptin on mouse trophoblast cell invasion. Biol Reprod 2004; 71:1963-1967.http://dx.doi.org/10.1095/biolreprod.104.032722
Jansson N, Greenwood SL, Johansson BR, Powell TL, Jansson T. Leptin stimulates the activity of the system A amino acid transporter in human placental villous fragments. J Clin Endocrinol Metab 2003; 88: 1205-1211.http://dx.doi.org/10.1210/jc.2002-021332
Turgut A, Ozler A, Goruk NY, Tunç SY, Sak ME, Evsen MS, Evliyaoglu O, Gul T. Serum levels of the adipokines, free fatty acids, and oxidative stress markers in obese and non-obese preeclamptic patients. Clin Exp Obstet Gynecol. 2015; 42:473-479.
Henson MC, Castracane VD. Leptin in pregnancy: an update. Biology of Reproduction 2006; 74:218-229. http://dx.doi.org/10.1095/biolreprod.105.045120
Rahardjo B, Widjajanto E, Sujuti H, Keman K. Different levels of IL-1α, IL-6, TNF-α, NF-κB and PPAR-γ in monocyte cultures exposed by plasma preeclampsia and normotensive pregnancy. Pregnancy Hypertens. 2014; 4:187-193. http://dx.doi.org/10.1016/j.preghy.2014.03.001
Kaartokallio T, Cervera A, Kyllönen A, Laivuori K. Gene expression profiling of pre-eclamptic placentae by RNA sequencing.Adicionalmente. Sci Rep. 2015; 5:14107. http://dx.doi.org/10.1038/srep14107
Challier JC, Uzan S. The human placenta and its pathologies: focus on oxygen. Med Sci (Paris). 2003; 19(11):1111-1120. http://dx.doi.org/10.1051/medsci/200319111111
Louwen F, Muschol-Steinmetz C, Reinhard J, Reitter A, Yuan J. A lesson for cancer research: placental microarray gene analysis in Preeclampsia. Oncotarget. 2012; 3(8): 759-773. http://dx.doi.org/10.18632/oncotarget.595
Redman C. The six stages of pre-eclampsia. Pregnancy Hypertens. 2014; 4(3):246. http://dx.doi.org/10.1016/j.preghy.2014.04.020
Torrado J, Farro I, Zócalo Y, Farro F, Sosa C, Scasso S, Alonso J, Bia D. Preeclampsia Is Associated with Increased Central Aortic Pressure, Elastic Arteries Stiffness and Wave Reflections, and Resting and Recruitable Endothelial Dysfunction. Int J Hypertens. 2015; 2015:720683. http://dx.doi.org/10.1155/2015/720683
Reyna-Villasmil E, Brice-o-Pérez C, Torres-Cepeda D. Inmunología, inflamación y Preeclampsia. Revista de Obstetricia y Ginecología de Venezuela. 2009; 69(2): 97-110.
Devergne O, Coulomb-L'Herminé A, Capel F, Moussa M, Capron, F. Expression of the Epstein-Barr virus-induced gene 3, an interleukin-12 p40-related molecule, throughout human pregnancy: involvement of syncytiotrophoblasts and extravillous trophoblasts. The American Journal of Pathology. 2001; 159(5): 1763-1776. http://dx.doi.org/10.1016/S0002-9440(10)63023-4
Van Der Hoorn ML, Keijser R, Ris-Stalpers C, Afink G, Claas FH, Van Der Post JA et al. Increased EBI3 expression in placentas of preeclamptic patients. Journal of Reproductive Immunology. 2010; 81: 1-61. http://dx.doi.org/10.1016/j.jri.2010.06.129
Guo J, Tian T, Lu D, Xia G, Wang H, Dong M. Alterations of maternal serum and placental follistatin-like 3 and myostatin in pre-eclampsia. Journal of Obstetrics and Gynecology Research. 2012; 38(7): 988-996. http://dx.doi.org/10.1111/j.1447-0756.2011.01823.x
Kleinrouweler CE, Van Uitert M, Moerland PD, Ris-Stalpers C, Van der Post JAM, Afink GB. Differentially expressed genes in the Pre-eclamptic placenta: A systematic review and meta-analysis. PLoS ONE. 2013; 8(7): e68991. http://dx.doi.org/10.1371/journal.pone.0068991
Dijke PT, Arthur HM. Extracellular control of TGF_ signaling in vascular development and disease. Nature Reviews. 2007; 8: 857-869. http://dx.doi.org/10.1038/nrm2262
Lowe SA, Bowyer L, Lust K, McMahon LP, Morton M, North RA, Paech M, Said JM. SOMANZ guidelines for the management of hypertensive disorders of pregnancy 2014. Aust N Z J Obstet Gynaecol. 2015; 55(5):e1-e29. http://dx.doi.org/10.1111/ajo.12399
Enquobahrie DA, Meller M, Rice K, Psaty BM, Siscovick DS, Williams MA. Differential placental gene expression in preeclampsia. American J Obstetrics & Gynecology 2008; 199:566.e1-566.e11. http://dx.doi.org/10.1016/j.ajog.2008.04.020