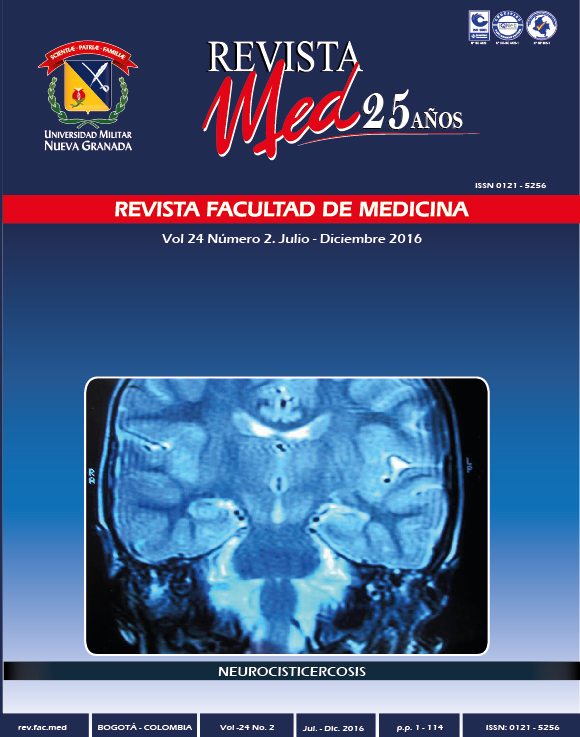
Symptoms associated with neurocysticercosis in people in the urban nd peri-urban of the municipality of coyaima the department of tolima and possible associated variables
Abstract
Introduction: The complex teniasis/cysticercosis is a worldwide public health problem. Colombia epidemiological studies shows the presence of parasites in humans resulting in neurocysticercosis (NCC).
Objective: To determine the symptoms associated with neurocysticercosis in people in the urban and peri-urban area of the town of Coyaima in the Department of Tolima and possible associated variables.
Materials and methods: a descriptive cross-sectional study was performed in the inhabitants of the urban and peri-urban area of the town of Coyaima in the Department of Tolima, who socialized informed consent. The 159 people that they agreed to participate voluntarily, is filled them a structured epidemiological survey, 5ml of blood making peripheral and simultaneously by finger stick blood collected in 4mm diameter filter paper circles; Similarly be asked a coprological sample that was set with MIF reagent to 5% and was processed with the concentration of formol-eter technique and finally stored at 4°C. Serologic evaluation, used the ELISA technique under the following parameters: Antigen fraction of 53kDa of the metacestodo of Taenia solium.; concentration of 0,4μg/ml, dilution of serum and whole blood taken with filter1/1, total serum conjugated 1/2500 and 1/100 paper. Statistical analysis included calculation of frequencies and Chi square 2 x 2 contingency tables.
Results: Of 159 participants, 17%(27/159) were diagnosed positive, and of these, 67%(18/27) presented any symptoms of possible partnership with NCC. Symptoms of greater frequency in the population studied were: headache, 19.5%; decrease of visual acuity, 5.7%; late-onset seizure, 4.4%; accidents cerebrovascular and alteration of consciousness 1.3% and 0.6%; respectively. Confirmed four people with NCC, of the positive Group(4/27) three female and one male, by techniques such as tomography Axial-TAC or magnetic resonance-MRI Imaging. The symptomatology of greatest relevance for these patients was seizure of late-onset and headache. The overall prevalence of intestinal parasitism in the participant population was 43.3%, identified in the 2%(3/159) rated, eggs of Taenia spp.; and of these a person positive turn, with symptoms (seizure of late-onset and headache) compatible with NCC and subsequent confirmation by TAC, suggesting a mixed parasitic infections by the adult stage and the metacestodo of T. solium.; in the patient.
Conclusions: 17%(27/159) of the studied population was positive, four persons were confirmed by imaging with NCC, whose symptoms of greater importance were seizure of late-onset and headache. The feminine gender is prone to suffer parasitosis. We found the presence of eggs of Taenia. spp.; in 2% of the population participating in the study. The variable sources of water for consumption presented statistical significance p≤ 0.05.
Downloads
References
Flórez A, PA, Salamanca L, Pastrán S, Vargas N, Beltrán M., Enríquez Y, Pe-a A, Villareal, Rincón C, Garzón I, Mu-os L, Guasmayan L, Valencia C, Parra S. Cisticercosis en Colombia. Estudio de seroprevalencia 2008-2010. Acta Neurológica Colombia. 2012; 29(2):73-85. Disponible en: http://www.scielo.org.co/pdf/anco/v29n2/v29n2a03
Nogales J, Arriagada C, Salinas R. Tratamiento de la Neurocisticercosis: Revisión crítica. Rev Méd Chile. 2006;134:789-796. Disponible en: http://www.scielo.cl/pdf/rmc/v134n6/art17.pdf
Flisser, A. Cisticercosis: enfermedad desatendida. Bol Med Hosp Infant Mex. 2011; 68(2):138-145. Disponible en: http://www.scielo.org.mx/scielo.php?script=sci_arttext&pid=S1665-11462011000200010
Vásquez L, Giraldo J, Agudelo P, Campo V, Vergara D. Experiencia para el control de la cisticercosis en el departamento del Cauca. Biomédica. 2011; 31 (3): 300-315. Disponible en: http://www.revistabiomedica.org/index.php/biomedica/article/viewFile/536/665
Flisser A, Sarti E, Lightowlers M, Schantz P. Neurocysticercosys, regional status, epidemiology, impact and control measures in the Americas. Acta Trop. 2003; 87:43-51. Disponible en: http://www.ncbi.nlm.nih.gov/pubmed/12781377 Fecha de consulta: 29/03/2016
Naquira C. Las zoonosis parasitarias: Problema de salud pública en el Perú. Revista peruana de Medicina Experimental y Salud Publica. 2010;27(4): 494-497. Disponible en: http://www.redalyc.org/articulo.oa?id=36318511001
U.S. Departament of healt and human services. Recommendations of the international Task Force for Disease Eradication. 1993; 42(RR-16). Disponible en: http://www.cdc.gov/mmwr/PDF/rr/rr4216.pdf
Walteros D. Cisticercosis: situación de parasitosis. Informe Final de Evento Cisticercosis. 2009. Disponible en: http://www.ins.gov.co/lineas-de-accion/Subdireccion-Vigilancia/Informe%20de%20Evento%20Epidemiolgico/Cisticercosis%202009.pdf
Giraldo J, Piraguata M, Bachiller Neiffe M. Estandarización de una prueba inmunodiagnóstica ELISA para la detección de anticuerpos humanos contra el metacéstodo de Taenia solium.; en extracto crudo y fracción proteíca de 53 kDa. Biomédica. 2002;22(s1):63.
Andriamandimby J, Heraud L, Randrianasolo T, Rafisandratantsoa S, Andriama- Monjy V, Reichard. Dried-blood spots: a cost- effective field method for the detection of chikungunya virus circulation in remote areas. Internacional Journal for Parasitology: Parasites and Wildlife. 2013;3:15-19. Disponible en:http://journals.plos.org/plosntds/article?id=10.1371/journal.pntd.0002339
Thangavelu A, Dhinakar R, Elankumaran S, Koteeswaran A. Evaluation of a filter paper blood sampling technique for quantitative assessment of antibodies to infectious bursal disease virus. Tropical Health and Production. 2000;32:179-182. Disponible en: http://link.springer.com/article/10.1023%2FA%3A1005239816285?LI=true#page-2
Flisser A, Plancarte A, Avila G. Application of diagnostic methods for cysticercosis and taeniosis to epidemiological studies. In: Taenia solium: Taeniasis/cysticercosis. Ed. Universo, Lima, Perú. 1999: 39-52.
Mahanty S, García HH. Cysticercosis Working Group in Perú. Cysticercosis and neurocysticercosis as pathogens affecting the nervous system. Prog Neurobiol.2010; 91:172-184. Disponible en: http://www.sciencedirect.com/science/article/pii/S0301008209002020
Montero J, Rojas R. Estudio retrospectivo de la seroprevalencia de neurocisticercosis en Colombia dentro del periodo de enero de 1995 a diciembre de 2005. Trabajo de grado bacteriología. Bogotá: Pontificia Universidad javeriana. Facultad de ciencias. Departamento de bacteriología. 2006:110-118. Disponible en: http://www.javeriana.edu.co/biblos/tesis/ciencias/tesis170.pdf
Franco C, Giraldo J, Vásquez R. Detección de anticuerpos anticisticerco en pacientes que asistieron a consulta médica durante el periodo 2009 a la Liga Contra la Epilepsia. Capitulo Cauca, Revista UNINCCA. 2012;18(1):79-93. Disponible en: https://www.unincca.edu.co/images/stories/pfd/revista-cientifica-v18-1.pdf
Ayala ER, Medina SA, Morales JA. Cisticercosis humana y sus asociación con factores epidemiológicos y clínicos en los Andes centro y sur de Perú. Revista epidemiológica del Perú. 2014;18(1):1-6 Disponible en: http://www.redalyc.org/pdf/2031/203131355005.pdf
Sotelo J. Controversias y perspectivas en Neurocisticercosis. En: Cisticercosis: Guía para profesionales de la salud. Ed fondo de Cultura económica, México. 2006;capVIII: 238-244. Disponible en:
Cortez M, Aguilar C, Rojas G, Boggio G., Lares M, Ferrer E, Parkhouse M. Evidencia de transmisión activa de cisticercosis por Taenia solium en comunidades rurales de Venezuela. Revista Biomédica. 2011;31(s3):300-315.
Agudelo S, Gómez L, Coronado X, Orozco A, Valencia C, Restrepo L, Galvis L, Palacio L. Prevalencia de parásitos intestinales y factores asociados en un corregimiento de la Costa Atlántica Colombiana. Revista de salud pública. 2008;10 (4): 633-642. Disponible en: http://www.scielosp.org/scielo.php?script=sci_arttext&pid=S0124-00642008000400013
Fica A, Castro M, Sotoa, Flores C, Oelker C, Weitzel T. Neurocisticercosis – una enfermedad desatendida en Chile. Revista Chil Infect. 2012;29(1): 72- 81. Disponible en: http://scielo-test.scielo.cl/pdf/rci/v29n1/art12.pdf
Takayanagui OM, Jardim E. Aspectos clínicos da neurocisticercose: analise de 500 casos. Arq Neuropsiquiatr. 1983; 41:50-63. Disponible en: http://www.scielo.br/pdf/anp/v41n1/04.pdf
Sato M. Cisticercosis, un obstáculo para el desarrollo: la situación en Brasil. Biomédica. 2011;31(3):300 -315. Disponible en: http://www.revistabiomedica.org/index.php/biomedica/article/viewFile/543/672
Mendes E, Santos da Silva S & La Terza Fonseca E, Regina Ribeiro de Souza Raimundo, Wilson de Carvalho. A neurocisticercose humana na Baixada Fluminense, Estado de Rio de Janeiro, Brasil. Arq. Neuro-Psiquiatr. 2005;63(4). Disponible en: http://www.scielo.br/scielo.php?script=sci_arttext&pid=S0004-282X2005000600027
Flisser A. Control de la teniasis y la cisticercosis en México, Biomédica. 2011;31(s3): 300-315. Disponible en: http://www.revistabiomedica.org/index.php/biomedica/article/viewFile/536/665
Del Brutto OH. Neurocisticercosis: actualización en diagnóstico y tratamiento. Rev. Neurología. 2005;20(8): 412-418. Disponible en: http://clinicalevidence.pbworks.com/w/file/fetch/77449862/Neurocisticercosis%20actualización%20en%20diagnostico%20y%20tratamiento.pdf.
Aluja A, Suarez R, Sciutto E, Biom I, Morales J, Veter D, Martínez J, Villalobos N. Evaluación del impacto de un programa de control de teniasis-cisticercosis Rev. Salud publica México. 2014;56(3):259-265. Disponible en: http://www.scielo.org.mx/scielo.php?script=sci_arttext&pid=S0036-36342014000300011